Overview of Immunotherapy Types for Drug Therapy
Immunotherapy is an umbrella term for any treatment that incorporates elements of the immune system to fight cancer. AIM with Immunotherapy broadly defines immunotherapeutic agents as drugs that alter the immune system response, regenerate immune recognition of foreign antigens, interfere with checkpoint controls, and/or comprise molecules stemming from the natural immunology.
What Types of Immunotherapies Have Been Approved to Treat Cancer?
The FDA has approved a wide range of these therapies, including immune checkpoint inhibitors, monoclonal antibodies, cytokines, CAR T-cell therapy, antibody-drug conjugates, and vaccines. By either enhancing or suppressing immune system responses, immunotherapy helps to regenerate immune recognition of cancer cells, interfere with checkpoint controls, and leverage the body’s natural immunology to target tumors.
Types of Immunotherapy:
- Antibody-Drug Conjugates
- Bispecific Antibodies
- Bispecific T-cell Engagers
- CAR T-Cell Therapy
- Cytokines/Immune System Modulators
- Immune Checkpoint Inhibitors
- Monoclonal Antibodies
- Tumor-Infiltrating Lymphocytes
- Vaccines
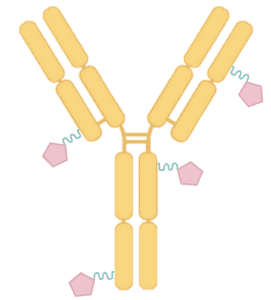
Antibody-drug conjugates or ADCs
A drug which combines a monoclonal antibody that recognizes a cancer antigen and is linked to a molecule of chemotherapy. After the antibody binds to the cancer cell expressing the antigen on its surface, the drug is internalized into the cell where it becomes unlinked, and releases the chemotherapy. The chemotherapy kills the cancer cell.
It is important to note that antibody-drug conjugates are sometimes organized into their own class of anticancer therapeutics. Here, they are loosely included on this website for two reasons: First, they rely upon antibodies for their efficacy which also differentiates these drugs from classic cytotoxic chemotherapy used in the 1950s; second, they represent a newer alternative class of agents that has over a dozen successful approvals thus far and deserves to be included in medical education.
Example: fam-trastuzumab deruxtecan and tisotumab vedotin-tftv
Bispecific Antibodies
A type of drug that consists of an antibody with two different binding domains that allows the antibody to recognize two different antigens in the molecular environment. This innovation categorizes bispecific antibodies as the “next generation” of development in monoclonal antibodies, an early concept utilizing knowledge from the immune system. Currently bispecific antibodies are used more often for hematological malignancies because they are less effective against solid tumors. Note that the terminology “bispecific antibodies” is often used synonymously with “bispecific t-cell engagers” or “bispecific T-cell engaging antibody” although there is a subtle difference in the construction, but it is not widely appreciated and may not be relevant to distinguish the broad function of these drugs, which pull T-cells and cancer cells together.
Example: amivantamab-vmjw and epcoritamab-bysp (considered a “bispecific T-cell engaging antibody”)
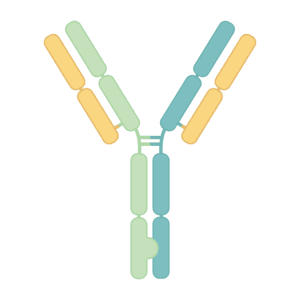
Bispecific T-cell Engagers
Considered to be a type of bispecific drug entity that characteristically brings an immunological T-cell to a tumor cell. Although it binds with one arm of the antibody to the tumor antigen, to distinguish it from being molecularly analogous to a bispecific antibody, the other arm could be a structure or other component, but not an antibody fragment. The non-antibody component binds specifically to an antigen on a T-cell, usually the CD3 subunit of the T cell receptor complex. This property makes bispecific T-cell engagers technically bispecific molecules since both arms of the drug entity are not antibody fragments. Bispecific T-cell engagers enhance the immune response by directing the T-cells to the cancer cells.
Example: talquetamab-tgvs, tebentafusp-tebn, and teclistamab-cqyv
Chimeric antigen receptor (CAR) T-Cell Therapy
A type of cell therapy whereby T lymphocytes are genetically engineered to express a receptor (i.e. the chimeric antigen receptor) that binds to an antigen on the cancer cell. The recognition of the cancer cell by the T cell through this receptor-antigen binding interaction results in the activation of the lymphocyte and elimination of the cancer cell. CAR T-cell therapy is currently approved for use in hematological malignancies such as B-cell acute lymphoblastic leukemia, chronic lymphocytic leukemia, follicular lymphoma, large B-cell lymphoma, mantle cell lymphoma, and multiple myeloma. Note that the T-cell therapy afamitresgene autoleucal approved for advanced synovial sarcoma is technically considered a cellular therapy.
Example: axicabtagene ciloleucel, ciltacabtagene autoleucel, and tisagenleucel
Cytokines or Immune System Modulators
Cytokines are small protein signals secreted by cells that send communications to, and then elicit responses from, the immune system by binding to a receptor.
The actions from specific cytokines can initiate (e.g. TNF, IL-6, etc.) or quiet (e.g. IL-1RA, TGF-beta, etc.) an inflammatory response. All of these can be manufactured as drug therapy for different reasons. Other types of molecules that belong to the broad class of cytokines includes chemokines, colony-stimulating factors, and interferons. “Superkines” are engineered cytokines that reduce the multiple effects of a cytokine to cause a specific action or enhance a signaling property.
Note that natural cytokines differ from hormones because hormones are chemical messengers secreted by specialized glands in the body. Cytokines can be secreted from adipose cells, immune cells, endothelial cells, or epithelial cells to impact the surrounding cells or tissues.
Example: IFNα2b and interleukin-2 (IL-2)
Immune Checkpoint Inhibitors or ICIs
The most popular type of immunotherapy for the number of indications and the responses achieved in treatment. Immune checkpoint inhibitors are monoclonal antibodies that bind to the programmed death receptor-1 (PD-1), programmed death receptor ligand-1 (PD-L1), or cytotoxic T-lymphocyte associated protein 4 (CTLA-4). PD-1, PD-L1, and CTLA-4 are involved in the negative regulation of the immune response. Engaging these will turn the immune response off, essentially acting to prevent an excessive immune reaction and potentially lethal autoimmune response. For this reason, PD-1 and other regulators acting in this manner are known as immune checkpoints. Since tumors engage immune checkpoints, selective binding by a monoclonal antibody blocks the engagement, prevents the shut off, and therefore allows the immune response to recognize the cancer cells. The recognition and resulting reactivation eliminates the cancer cells.
Example: ipilimumab, nivolumab, and pembrolizumab
Monoclonal Antibodies
A laboratory-engineered immunoglobulin or Y-shaped molecule that will recognize and bind to one antigen or epitope only, even though antibodies have the ability to recognize more than one antigen or epitope. As a drug entity, a monoclonal antibody will bind to a molecular target, which is often a receptor site and block an interaction from occurring. Often, this interaction is based on an oncogenic addiction of the cancer cell that is required for the cancer to thrive. Alternatively, a monoclonal antibody could bind to a specific molecule found abnormally abundant on the cancer cell (e.g. BCMA, CD19, CD20, etc.) and act as a red flag to elicit antibody-dependent cell-mediated cytotoxicity. This is an adaptive immune response that occurs when immune cells recognize antibody-coated cancer cells and trigger cell lysis. The result is the elimination of the red-flagged cancer cell by the immune system. Note that monoclonal antibodies are also considered “targeted therapies.”
Example: isatuximab-irfc and tafasitamab-cxix
Oncolytic Virotherapy
A type of treatment that genetically modifies a natural human virus to target and infect cancer cells. After infection, the virus multiplies itself within the cancer cell, replicating to large numbers that will eventually cause oncolysis, the process whereby a cancer cell bursts open and spills out its contents. Oncolysis releases newly-replicated viruses to infect neighboring cancer cells and releases tumor-associated antigens that can stimulate an immune response. Alerting and recruiting immune cells to the site of infection re-energizes an attack on cancer cells.
Example: talimogene laherparepvec (T-VEC)
Tumor Infiltrating Lymphocyte (TIL) therapy
A type of cell therapy that surgically removes part(s) of a tumor and the localized immune cells within the tumor. The effective immune cells are extracted from the tumor and expanded in a certified laboratory. The abundant immune cells are then reintroduced back into the patient. The result gives the patient’s immune system a much larger, effective immune cell population that works to eliminate cancer cells. Note that this type of therapy has multiple steps to the therapeutic regimen, which includes the use of an interleukin as well as chemotherapy. It is also different from CAR T-cell therapy which genetically alter cells to express a chimeric antigen receptor, whereas TIL therapy does not.
Example: lifileucel
Vaccines
A drug process whereby tiny attenuated virus particles are introduced into the body to educate the immune system on identification and response. This education is necessary to generate antibodies that will specifically identify the viral antigens, without threat of a lethal infection. In this way, the immune system will now be able to recognize the same viral antigens in the future from a real viral infection. If the virus entered the system and infected cells, then the immune system would recognize the virus particles and respond by quickly flagging infected cells with the antibodies from memory. This rapid identification allows the immune cells to eliminate the threat by killing infected host cells.
Example: bacillus Calmette–Guérin and human papillomavirus 9-valent vaccine