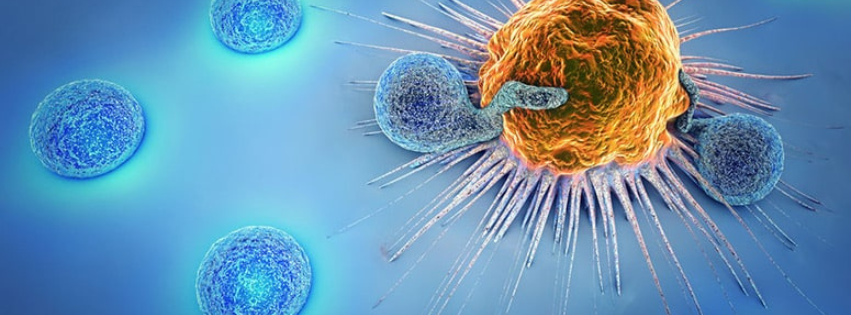
Helping an individual’s immune system to re-recognize and identify cancer cells has proven to be the most effective drug strategy thus far for treating cancer. In comparison to chemotherapy, targeted small-molecule inhibitors, and hormonal agents, immunotherapy has a superior ability to achieve a state of non-existent disease when it is effective.
In this way, immune checkpoint inhibitors (ICIs) can have a substantial impact against various cancer types. Initially, immunotherapy was discovered for melanoma, which had no other reliable options for drug therapy before 2011. After that time, targeted therapy and immunotherapy became the mainstay of treatment for melanoma.
However effective they may be, ICIs come with challenges. Since they broadly and nonspecifically activate the immune system, they also cause inflammation throughout the body, which affects every organ system. Their unfortunate ability to elicit immune-related adverse events (irAEs) in a majority of patients (~81.0%) often requires drugs to counteract that response.
Without quelling the inflammation produced by the immune system, the reaction could become life-threatening. Approximately 70% of patients will have mild irAEs, and 20% will have severe irAEs. For these reactions, corticosteroids and/or additional immunosuppressants are administered to the patient. They work by blunting the immune response, which is also the anti-tumor response.
Outcomes with Steroid Use
Although there is conflicting evidence on the impact of steroid use among patients treated with immune checkpoint inhibitors (ICIs), a recent study suggests progression-free survival (PFS) and overall survival (OS) are not impacted. Data collected by the Massachusetts General Hospital in Boston and the Vanderbilt Ingram Cancer Center in Nashville shows that whether or not patients on ICIs received steroids, their outcomes will not change.
These results convey excellent news for those who have immune-related adverse events (irAEs) during treatment. Even better news is that both PFS and OS significantly increased among patients who experienced irAEs compared to the patients who did not. In other words, having side effects comes with a silver lining.
Among 226 patients treated with the combination of ipilimumab and nivolumab for advanced melanoma, those experiencing irAEs of any grade had a median PFS of 18.4 months, compared to 1.2 months in patients who did not experience irAEs (p < 0.0001). Similarly, patients had a median OS of 51.8 months if they experienced irAEs versus 4.9 months if they did not experience irAEs (p < 0.0001).
Outcomes Related to Steroid Induction
| Response Rates | Time to Steroid Use | Patients |
| 32.5% | 0 – 28 days | 40 |
| 50.0% | 28 – 49 days | 30 |
| 65.6% | 49 – 70.2 days | 32 |
| 73.5% | 70.2 – 144 days | 34 |
According to the data presented, timing is related to outcome. For patients who experienced an irAE and were first exposed to steroids within 28 days of treatment, the median PFS was 5.36 months, and the OS was 23.6 months. For patients who were first exposed to steroids between 28-49 days after starting treatment, their median PFS was 7.84 months, and OS was 32.6 months.
If patients were exposed to steroids either 49-70 days or 70.2-144 days after initiating ICIs (ipilimumab and nivolumab), their PFS was not reached at 70.92 months, and the median OS was not reached, indicating that they were still surviving. Therefore, having a late inflammatory response suggests a better prognosis.
These responses and their timing also correlated with the response rates of these groups. With a shorter time to initiate steroids due to irAEs, 32.5% of patients responded to therapy. This is compared with 73.5% of patients responding to therapy when they had a longer interval between the initiation of ICIs and subsequent exposure to steroids. Taken together, the data suggest that a delayed reaction to ICIs results in improved outcomes.
Use of Additional Immunosuppressants and Peak Dose
Systemic corticosteroids are used in patients to quell most irAEs. However, when this approach is not practical, additional immunosuppressants are introduced. Data from this study suggests a correlation with outcomes if additional immunosuppressants are necessary.
| Nivolumab/relatlimab cohort results | ||
| Patients w/irAEs (n=25) | No irAEs (n=17) | |
| Response Rate | 60.0% | 11.8% |
| Median PFS | 31.5 months | 9.0 months |
| Median OS | 96.4 months | 19.3 months |
Among patients who required additional immunosuppressants, they experienced a poorer OS (p=0.018). The caveat to this finding was that the use of replacement steroid therapy for adrenal insufficiency was associated with improved OS (p=0.024).
The results of the study suggest there is also an association between higher peak steroid doses and patient outcomes. Poorer PFS (p = 0.005) and OS (p = 0.003) among patients correlated with a higher peak steroid dose in a subgroup analysis.
Since science is never reliant on a single study, the authors used a second cohort to test their conclusions. For this, 42 patients treated with nivolumab and relatlimab were analyzed to determine whether the findings would be the same or similar. There was no difference in patient outcomes based on peak steroid dose. The authors attributed this to the smaller patient numbers of this cohort.
Taken together, the data suggests there may be caveats to outcomes when steroids are necessary. However, when steroids are needed to counter an irAE, this will not significantly impact the response, PFS, or OS.
Conclusion
The combined results suggest that overall, patients who experience irAEs during treatment with ICIs will tend to have better outcomes than those who do not experience any irAEs. The findings seem logical, given that the mechanism of action for ICIs requires the generation of a non-specific response from the immune system, which could impact any organ system. A broad activation of the immune system is the anti-cancer mechanism that will destroy the tumor. Unwanted irAEs are likely to result if the drugs are working.
Having steroids to quell the immune response is essential when this occurs to prevent lapses in treatment, permanent discontinuation of ICIs, and poor outcomes for patients. Systemic corticosteroids should remain the standard treatment for moderate-to-severe irAEs, and the timing of their use should be recorded as a prognostic indicator of outcome.
This summary was based on the original research article, “Impact of steroid dose and timing on efficacy of combination PD-1/CTLA-4 blockade,” by Curkovic NB, et al. It was published in Oncoimmunology in 2025. doi: 10.1080/2162402X.2025.2494433.