TIL Therapy
How can you and your caregiver prepare for treatment with TIL therapy?
The recent approval of tumor-infiltrating lymphocyte (TIL) therapy—sometimes referred to as “TILs”—has generated questions about the treatment process for patients with melanoma. Here we explain the treatment details and patient experience. Although it may seem like an overly complicated, multi-step hospital procedure, we will break down the process and explain why it is designed this way. If you still have questions, reach out to us.
What is TIL therapy?
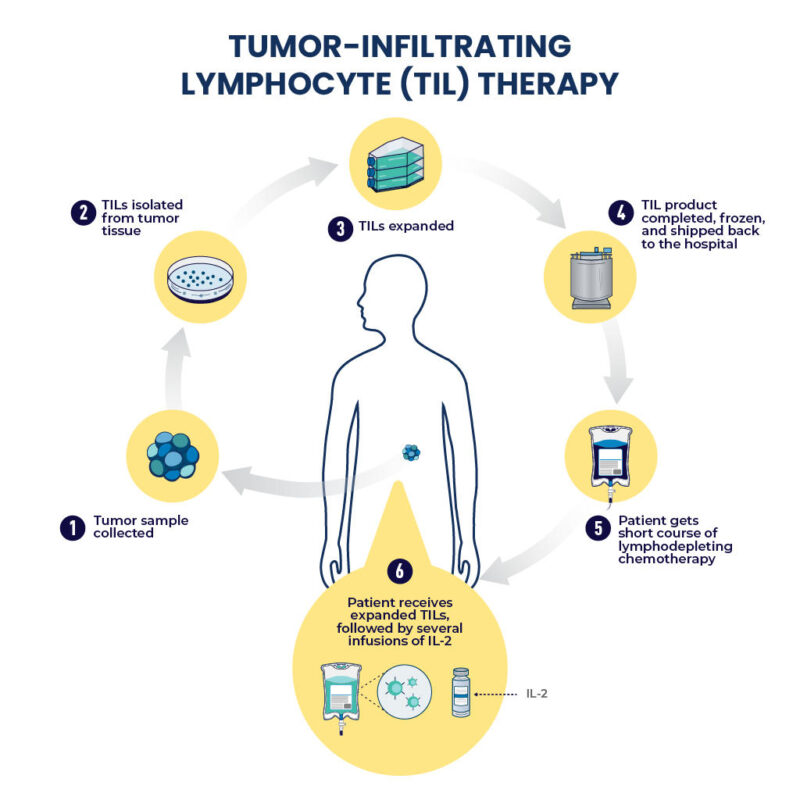
TIL therapy is a process in which the immune cells that are effective at fighting your cancer are removed from your body, grown and multiplied in a lab, and then reintroduced back into your body to better fight your cancer. The expanded number of targeted immune cells and the treatment process were approved by the FDA as lifileucel (Amtagvi).
In addition to the immune cell infusion process, TIL therapy includes the administration of two other drug regimens over the course of multiple weeks. Although TIL therapy may seem complex, multiple steps are required for the treatment to be effective. Expect to spend at least two weeks in the hospital if you undergo this type of treatment.
One other essential note: Patients largely display improved TIL therapy outcomes when they are treated earlier in their disease course. In other words, TIL therapy is not likely to be as effective as a fourth- or fifth-line treatment option versus second- or third-line. When patients are considering TILs, trying it earlier, after progression on immunotherapy, generally produces better outcomes. To be eligible for TILs, patients must have had at least one prior treatment with immunotherapy. For patients whose melanoma has a mutation in the BRAF gene, they must also have tried targeted therapy medications.
Drugs administered during hospital treatment
Overall, three drug milestones are required for successful TIL therapy: immune depletion, TIL administration, and TIL expansion. Each milestone includes the administration of a drug: chemotherapy, lifileucel, and interleukin 2 (IL2, which is also sometimes referred to as aldesleukin). Each step could take days or weeks, depending on you, your health status, and how well you tolerate each drug regimen milestone. Doctors emphasize that patients’ ability to achieve a good outcome is often a reflection of their health status when they check into the hospital. Therefore, maintaining healthy nutrition, adequate sleep, and exercising (if possible) before TIL treatment begins is important.
Chemotherapy
You will be given chemotherapy to prepare your body to receive TIL therapy. Although chemotherapy is typically given to shrink tumors and kill cancer cells, it is not given for these reasons prior to TIL therapy. The goal is not to treat the cancer. Instead, it prepares your body to receive your expanded immune cells. The chemotherapy eliminates the immune cells in your body; it may be called an “immune-depleting drug” or “lymphodepletion.” Eliminating your current immune cells allows the re-introduced tumor-specific immune cells to take hold in the blood and bone marrow when infused.
You will receive two chemotherapy drugs, cyclophosphamide and fludarabine. You will usually get two days of cyclophosphamide and five days of fludarabine. Some centers will administer chemotherapy in the hospital, and other centers will administer chemotherapy as outpatient therapy. That variation will affect the overall length of your TILs hospital stay.
The chemotherapy doses are not the typical doses that patients with other solid tumors receive for cancer. These are different chemotherapy medications than typically used, since they are not targeting the cancer and instead are targeting the immune system. If managed correctly, this chemotherapy should not cause extreme side effects, though all chemotherapy comes with risks. Prior to receiving chemotherapy, supportive medications are given to minimize unpleasant side effects. Although some patients may feel a little nauseous, many patients will not feel different after receiving the low-dose chemotherapy.
Unfortunately, the “immune-depleting” chemotherapy treatment causes hair loss days after it is administered. Patients will lose the hair on their bodies while they are in the hospital. Hair will start to regrow weeks after chemotherapy is finished, but it sometimes returns in a different color or texture. Patients will also have to wear a mask if they leave their hospital room and for a period of weeks because their immune system is depleted.
Tumor-infiltrating lymphocytes (TILs)
The day after the chemotherapy is completed, you will receive your infusion of TIL cells, also called lifileucel. You will be hospitalized for this portion of the treatment. For this process, the nurse will connect a new IV bag for your new TIL cells to flow into your veins and blood system. Receiving the TILs is a short process that takes 60 to 90 minutes. You should feel fine during the administration, though some patients will experience chills.
Aldesleukin or interleukin 2 (IL-2)
After the TILs are infused, you will receive a drug called aldesleukin or interleukin-2 (IL-2) in your IV. This drug stimulates the immune cells and causes them to replicate or make more of themselves. In this instance, the IL-2 will signal to your TIL cells to increase their abundance. Receiving IL-2 to magnify the number of T-cells is an essential part of your treatment. The new T-cells must multiply quickly to form an elite army to attack the melanoma. These cells have been selected based on specific properties that will enable them to work very well against your cancer.
The IL-2 drip is usually given in your hospital room. At some hospitals, patients are transferred to the intensive care unit for closer monitoring when they receive an IL-2 drip but this is typically not needed. This drug has been around for a while to treat melanoma and kidney cancer, and its side effects are well known, but it can be dangerous. Specially trained and prepared medical teams manage patients receiving IL-2 to reduce the risk of complications.
Depending on how well you tolerate high-dose IL-2, you could receive between one and six doses. It is given either every eight or twelve hours depending on the hospital protocol. During those days, you will be checked by the hospital health care providers multiple times each day. The staff will monitor vital signs and take blood samples to measure your health status. These checks ensure that you remain healthy and it is safe to receive another dose of IL-2. Each dose signals to the immune system to create more TIL cells.
Expectations during the hospital stay
You should expect to spend around two weeks in the hospital for your entire TILs treatment, but every patient is different. Your healthcare providers will communicate with you about each drug milestone during this time. A provider will visit your room at least once daily to review your lab results and go through a physical exam. The providers are required to ensure that it is safe to proceed with the next drug dose and the next steps.
 Healthcare providers will communicate what will happen each day. The providers around patients with TILs want to ensure that someone responds promptly to questions or side effects that may occur. They want to get on top of things quickly, and they do not want patients to have a lot of side effects.
Healthcare providers will communicate what will happen each day. The providers around patients with TILs want to ensure that someone responds promptly to questions or side effects that may occur. They want to get on top of things quickly, and they do not want patients to have a lot of side effects.
Patients and caregivers must know that no provider feels burdened by patients. Sometimes you may feel like you are taking up too much of the provider’s time, and on occasion, the feeling of burdening a provider can be a communication barrier.
If you have questions during your hospital stay, asking your provider for answers is important. Sometimes, having another person around can help with effective communication. You may get flustered when the medical team enters your hospital room. Having an advocate—such as your spouse, a friend, your son or daughter—in that setting can help. They can take notes, remind you of questions you have, and ask questions on your behalf.
Preparing for time in the hospital
Although each patient’s experience varies, expect to be in the hospital for about two to three weeks. Healthcare providers advise leaving work at home but bringing a laptop and other items that can help keep you entertained, as some days could be long and boring. Though some patients expect they will sleep the whole time because they will not feel well, most of the time patients feel really well – leading to boredom.
 Healthcare providers encourage patients to walk around their rooms or the hospital floor. Comfortable slippers are key for this activity. Providers have seen patients bring yoga mats and exercise mats so that they can stretch in their rooms. Some patients bring books to read and music to listen to. Cell phones and electronic chargers are especially important to remember. Other patients have started a blog post to communicate with supporters during their hospital stay.
Healthcare providers encourage patients to walk around their rooms or the hospital floor. Comfortable slippers are key for this activity. Providers have seen patients bring yoga mats and exercise mats so that they can stretch in their rooms. Some patients bring books to read and music to listen to. Cell phones and electronic chargers are especially important to remember. Other patients have started a blog post to communicate with supporters during their hospital stay.
Since patients are living at the hospital for a few weeks, providers encourage selecting comfortable garments from home. It may help to bring comfortable pajamas and PICC line shirts to avoid wearing a hospital gown the whole time. In addition, you might want to bring a favorite pillow for comfort.
Recently, some centers have encouraged patients to bring a comfort food with them, like alphabet soup or chicken noodle soup. The food should be what you usually eat when you do not feel well. Other centers may provide patients with a list of things to bring with them to the hospital, which will indicate whether bringing in outside food is allowed.
Lastly, it is important to ensure you have a support system in the hospital so you do not feel alone. You might arrange to receive daily phone calls from friends and family, as well as select visitors to your hospital room over the course of your treatment. Healthcare providers encourage patients to have plans that include connecting with people.
Expectations after leaving the hospital
 Congratulations on ringing the bell and being wheeled outside your healthcare facility! You should celebrate completing TIL therapy treatment. Medical criteria for hospital discharge are that your baseline immune system has come back to a safe level and does not require antibiotics. In addition, you must have recovered from major side effects experienced with treatment.
Congratulations on ringing the bell and being wheeled outside your healthcare facility! You should celebrate completing TIL therapy treatment. Medical criteria for hospital discharge are that your baseline immune system has come back to a safe level and does not require antibiotics. In addition, you must have recovered from major side effects experienced with treatment.
It is important to note that patients are still weakened when they leave the hospital. You will be given discharge instructions with contact numbers of your healthcare providers. You will likely be discharged from the hospital with some prescriptions and medicine to continue taking and might also be prescribed some precautionary medication.
While the protocols differ between hospitals, patients are typically seen at the clinic multiple times a week until they reach approximately 30 days after TILs infusion to be monitored for potential side effects. Providers plan scans at regular intervals based on the practice of their hospitals. Often the first scan is between 4 and 8 weeks after the TIL infusion. This scan is when response to treatment may become apparent.
The vital role for caregivers of patients receiving TIL therapy
Caregivers are always crucial parts of the cancer journey. Yet TIL therapy requires caregiving at a level that may be higher than other types of treatment. The support needed from caregivers starts from the day planning begins for TIL therapy and lasts throughout treatment. Caregivers need to have patience and an understanding that their role is to help get the patient through the treatment.
Taking care of the details is one of the most important things a caregiver can do to help the patient. A caregiver can keep records of every appointment, medication, and doctor on a cell phone. The benefit is that all of this information is available to pull up instantly if there are questions.
Managing the calendar becomes very important. It is ideal for a caregiver to help keep track of the medical appointments. Many tests must be done before TIL therapy. For example, a patient must have an ultrasound of the heart and many labs before approval for TIL therapy is granted. It gets more complicated once the medical team schedules the surgery, scans, and tests for TIL therapy. An organized caregiver who helps keep track of those dates can unburden a patient who may be feeling anxious.
 A supportive caregiver allows their loved one to be the patient. There could be substantial apprehension leading up to the hospital treatment, and providing emotional support is critical during that period. Once the patient is in the hospital, they will be surrounded by healthcare providers all day, as someone is present all the time in the hospital. In the lead-up period, however, patients may feel isolated, anxious, or stressed.
A supportive caregiver allows their loved one to be the patient. There could be substantial apprehension leading up to the hospital treatment, and providing emotional support is critical during that period. Once the patient is in the hospital, they will be surrounded by healthcare providers all day, as someone is present all the time in the hospital. In the lead-up period, however, patients may feel isolated, anxious, or stressed.
After treatment in the hospital, caregivers can help the patient get up and get moving. They can help the patient get outside if they are able to, depending on where the patient’s white blood cell count is. More importantly, caregivers who know the patient well are a second set of eyes for the clinicians. When caregivers notice that something is off, that is often the first notification that the clinician may get.
After the hospital stay, every clinic or hospital will have slightly different requirements, but some healthcare centers may follow CAR T-cell rules. Those rules include the requirement that a patient has a 24-hour caregiver present for approximately 30 days from their TIL cell infusion. This requirement is not an FDA requirement for TIL therapy, but some centers have incorporated it for safety. The cancer center will indicate whether this requirement is part of their process before your treatment, so you have time to plan for your caregiver. Usually, patients must remain within a one-hour drive of the hospital during that period in case of emergency complications.
Keep in mind that the caregiver does not need to be a medical person or a licensed health care provider. Caregivers are needed after the patient leaves the hospital in case the patient has an overnight fever, doesn’t feel well, or needs help with something. Some healthcare centers have a social worker who sees patients before the TIL process. The social worker will meet with the caregiver to lay out a caregiver schedule and describe how caregivers can best support patients.
In conclusion
If you are interested in TIL therapy, the first step is to speak with your healthcare provider. They will know whether you may be eligible for treatment. If you are eligible, they can refer you to an authorized TIL treatment center. These are clinics that are approved to treat patients with TIL therapy – not all facilities are able to do this. At these clinics, the staff will guide you through the process of eligibility, surgery for collecting a sample of your T-cells, and going through the entire process.
TIL therapy is a complicated process, but the multiple steps involved during the hospital stay are necessary to keep the patient safely managed through the critical treatment procedures. Clinical trials are underway to assess whether changes can be implemented into this process to reduce the length of time and steps currently required, but for now, expect the process explained on this page. Caregivers are an important part of the healthcare team for managing a patient with TILs, caring for a patient, and helping a patient with details, appointments, and other parts of the treatment process.
Additional Resources
The FDA Approval of TIL Therapy and What it Means for Advanced Melanoma
Written and Edited Transcript of Webinar on TIL Therapy
In Plain English: Tumor-Infiltrating Lymphocyte (“TIL”) Therapy for Advanced Melanoma
